Symptoms of plantar fasciitis
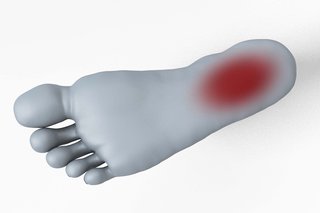
The main symptom of plantar fasciitis is pain on the bottom of your foot, around your heel and arch.
It's more likely to be plantar fasciitis if:
- the pain is much worse when you first start walking after sleeping or resting
- the pain gradually gets better when you start moving around, but gets worse if you stand, walk or run for a long time
- it's painful to stretch the bottom of your foot, for example when you raise your toes off the floor or walk up stairs
How to ease plantar fasciitis yourself
If you see a GP for plantar fasciitis, they'll usually suggest you try these things:
Do
-
rest and raise your foot on a stool when you can
-
put an ice pack (or bag of frozen peas) in a towel on the painful area for up to 20 minutes every 2 to 3 hours
-
wear shoes with cushioned heels and good arch support
-
use insoles or heel pads in your shoes
-
try regular gentle exercises to stretch the sole of your foot and your heel
-
try exercises that do not put pressure on your feet, such as swimming
-
take painkillers like paracetamol or ibuprofen gel, or ibuprofen tablets if you need them
-
try to lose weight if you're overweight
Don’t
-
do not walk or stand for long periods
-
do not wear high heels or tight pointy shoes
-
do not wear flip-flops or backless slippers
-
try not to walk barefoot on hard surfaces
A pharmacist can help with plantar fasciitis
You can ask a pharmacist about:
- the best painkiller to take
- insoles and pads for your shoes
- if you need to see a GP
Non-urgent advice: See a GP if:
- you have pain in the bottom of your foot that is severe or stopping you doing normal activities
- your foot pain is getting worse or keeps coming back
- your foot pain has not improved after treating it yourself for 2 weeks
- you have any tingling or loss of feeling in your foot
- you have diabetes and foot pain – foot problems can be more serious if you have diabetes
Treatment for plantar fasciitis from a foot specialist
If plantar fasciitis does not get better, a GP might refer you to a physiotherapist or foot specialist (podiatrist).
A physiotherapist can show you exercises to help ease your symptoms. A podiatrist can recommend things like insoles and the right shoes to wear, or splints to wear at night.
If these things do not help, a specialist may offer other treatments such as steroid injections, or using a machine to deliver high-energy sound waves to your foot (extracorporeal shock-wave therapy). Less commonly you may be offered surgery.
Physiotherapy is available free of charge on the NHS throughout the UK but waiting times for accessing physiotherapy can sometimes be long.
Podiatry may not be available for free on the NHS everywhere and waiting times can sometimes be long.
You can also pay to see a podiatrist or physiotherapist privately.
Self-refer for treatment
If you have plantar fasciitis, you might be able to refer yourself directly to services for help with your condition without seeing a GP.
To find out if there are any services in your area:
- ask the reception staff at your GP surgery
- check your GP surgery's website
- contact your integrated care board (ICB) – find your local ICB
- search online for NHS treatment for plantar fasciitis near you
Common causes of plantar fasciitis
Plantar fasciitis is caused by straining the part of your foot that connects your heel bone to your toes (plantar fascia).
It's not always clear why this happens.
Plantar fasciitis is common. You may be more likely to get it if you:
- are 40 to 60 years of age
- recently started exercising on hard surfaces
- exercise with a tight calf or heel
- overstretch the sole of your foot during exercise
- do a lot of standing, walking or running, or started doing a lot more than is usual for you
- wear shoes with poor cushioning or support
- are overweight
Page last reviewed: 14 February 2025
Next review due: 14 February 2028