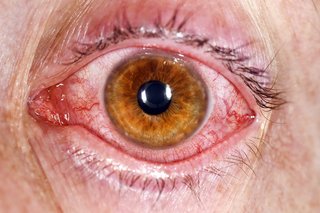
Check if you have conjunctivitis
Conjunctivitis is also known as red or pink eye.
It usually affects both eyes and makes them:
- red
- burn or feel gritty
- produce pus that sticks to lashes
- itch
- water


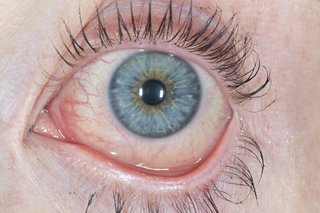
If you're not sure it's conjunctivitis
How to treat conjunctivitis yourself
There are things you can do to help ease the symptoms of conjunctivitis.
- Wash your eyelids with clean water. Boil the water and let it cool down, then gently wipe your eyelashes with a clean cotton wool pad to clean off crusts (1 piece for each eye).
- Hold a cold flannel on your eyes for a few minutes to cool them down.
Do not wear contact lenses until your eyes are better.
A pharmacist can help with conjunctivitis
Speak to a pharmacist about conjunctivitis. They can give you advice and suggest eyedrops or antihistamines to help with your symptoms.
If you need treatment for a child under 2 years old, you'll need a prescription from a GP.
Stop infectious conjunctivitis from spreading
There are things you can do to stop conjunctivitis spreading to other people.
Do
-
wash your hands regularly with warm soapy water
-
wash your pillow cases and face cloths in hot water and detergent
-
cover your mouth and nose when sneezing and put used tissues in the bin
Don’t
-
do not share towels and pillows
-
do not rub your eyes
Staying away from work or school
You do not need to stay away from work or school unless you or your child are feeling very unwell.
Non-urgent advice: See a GP if:
- your baby has red, sticky eyes – get an urgent appointment if your baby is less than 30 days old
- you wear contact lenses and have conjunctivitis symptoms as well as spots on your eyelids – you might be allergic to the lenses
- you have conjunctivitis and your symptoms have not cleared up within 7 days
Urgent advice: Ask for an urgent GP appointment or get help from NHS 111 if you have:
- pain in your eyes
- sensitivity to light
- changes in your vision, like wavy lines or flashing
- very red eyes (1 eye or both eyes)
- a baby less than 30 days old with red, sticky eyes
These can be signs of a more serious eye problem.
You can call 111 or get help from 111 online. Call 111 if you need help for a child under 5.
Treatment for conjunctivitis
Treatment will depend on the cause of your conjunctivitis.
If it's a bacterial infection, you might be prescribed antibiotics. But these will not work if it's caused by a virus (viral conjunctivitis) or an allergy.
Some sexually transmitted infections (STIs) can cause conjunctivitis. This type takes longer to get better.
Page last reviewed: 23 April 2024
Next review due: 23 April 2027